Why Regional Data Matters for Addiction Recovery
Regional data is the backbone of effective addiction recovery strategies. It highlights local trends, gaps in treatment access, and the unique challenges faced by specific communities. Without this level of detail, resources risk being misallocated, leaving critical issues unresolved. Here's why focusing on regional data is essential:
- Substance Use Varies by Region: For example, stimulants dominate in Western states, while opioids are more prevalent in Appalachia.
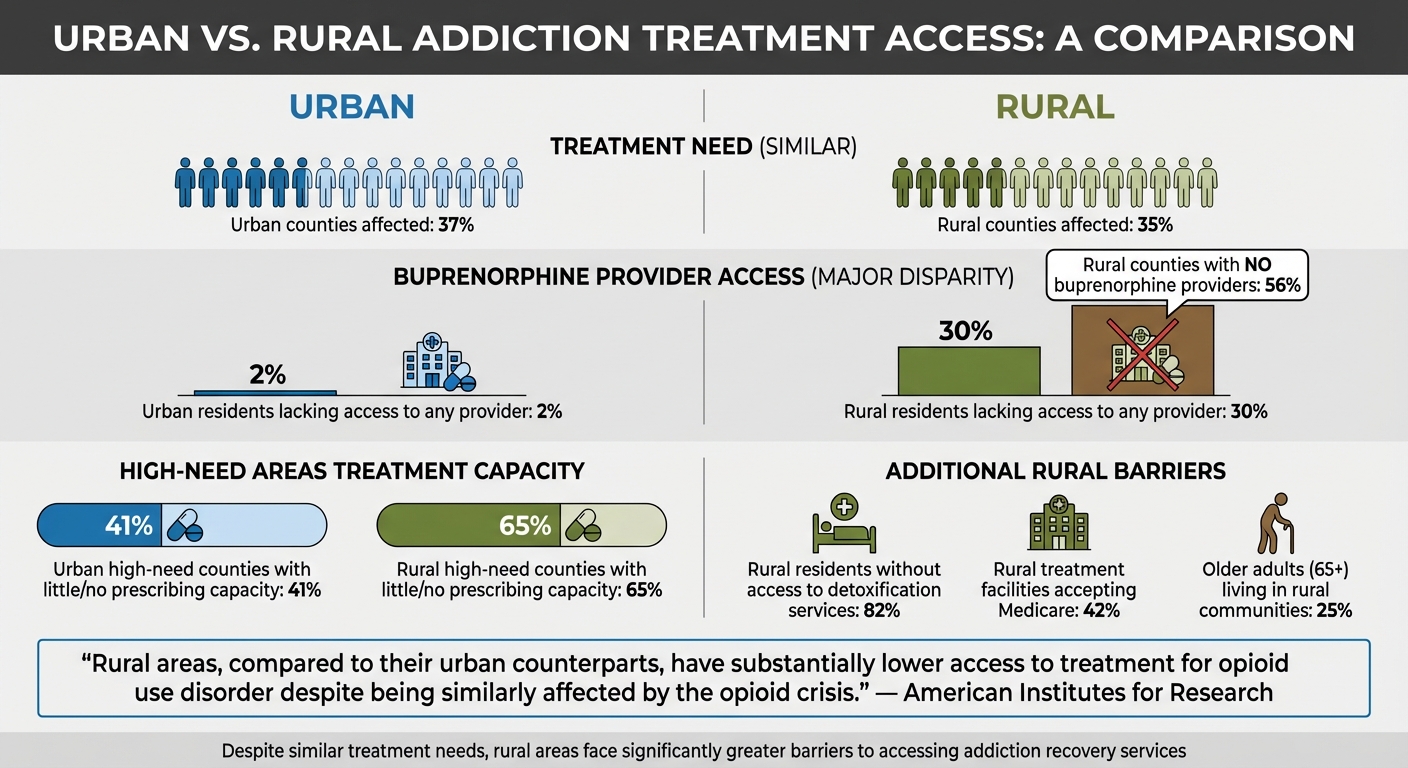
- Access Gaps: Rural areas face severe shortages in treatment options - 56% of rural counties lack providers for opioid treatments like buprenorphine.
- Demographic Disparities: Groups like American Indians in Minnesota face disproportionate overdose death rates compared to other populations.
- Localized Solutions Work: Programs tailored to specific needs, like West Virginia’s maternal care for substance-affected newborns, show measurable success.
The takeaway: Regional data helps pinpoint where intervention is needed most, ensuring recovery programs address the right problems in the right places.
Innovative treatments for drug addictions - New Day NW
How Addiction Patterns Differ by Region
Urban vs Rural Addiction Treatment Access Disparities
Geographic and Demographic Differences in Addiction
The substances driving addiction vary significantly depending on the region. While alcohol remains the leading cause of inpatient stays across the U.S., the second most common substance shifts geographically. For instance, in Western states like California and Hawaii, stimulants - especially methamphetamine - are the second most prevalent. In contrast, opioids dominate treatment admissions in the Northeast and Appalachia.
Some areas stand out with striking statistics. Baltimore City, Maryland, reported the highest urban rates of opioid-related inpatient stays between 2013 and 2015, with 1,592 stays per 100,000 people. Stimulant-related stays in the same city reached 931 per 100,000 people. On the other hand, Sioux County, North Dakota, a rural area, recorded the nation’s highest rate of alcohol-related inpatient stays - 2,725 per 100,000 population. In many rural regions, factors like high unemployment and incarceration rates further increase the risk of opioid overdose deaths. These regional differences highlight the importance of customized recovery strategies.
Treatment Access: Urban vs. Rural Areas
Although the need for opioid use disorder treatment is similar in rural and urban counties - affecting about 35% of rural and 37% of urban counties - access to treatment is far more limited in rural areas. For example, 56% of rural counties don’t have a single provider authorized to prescribe buprenorphine, a key medication for treating opioid use disorder. In rural areas, 30% of residents lack access to any buprenorphine provider, compared to just 2% in urban areas.
"Rural areas, compared to their urban counterparts, have substantially lower access to treatment for opioid use disorder despite being similarly affected by the opioid crisis." - American Institutes for Research
The disparity is even more pronounced in high-need areas. Among rural counties with the greatest demand for treatment, 65% have little to no capacity for buprenorphine prescribing, while this figure drops to 41% in high-need urban counties. Beyond medication access, 82% of rural residents live in counties without detoxification services. Medicare acceptance also poses a challenge, as only 42% of treatment facilities in rural areas accept Medicare, which is critical for the 25% of older adults living in these communities. These gaps in access underline the need for targeted solutions.
How Community and Culture Affect Recovery
Local culture and community dynamics play a major role in recovery outcomes. In rural areas, tight-knit communities can amplify stigma, discouraging individuals from seeking treatment. Transportation is another hurdle, as limited public transit and the loss of driver’s licenses make it difficult for many rural residents to reach treatment facilities.
Some communities have created programs tailored to their unique needs. The Seneca Nation’s Seneca Strong program, for instance, employs Certified Addiction Recovery Coaches to deliver peer advocacy designed specifically for their community. Similarly, West Virginia’s DrugFree Moms and Babies program was developed in response to rising cases of neonatal abstinence syndrome. This initiative provides early intervention and standardized clinical care for pregnant women and their newborns. These examples show how recovery efforts can benefit from addressing the specific cultural, economic, and geographic challenges each community faces. By understanding and adapting to these local factors, programs can better support individuals on their path to recovery.
Using Technology to Collect and Analyze Regional Data
How Recovery Center CRM Collects Regional Data
Modern CRM systems have transformed how recovery programs manage data, addressing the inefficiencies of fragmented, paper-based record-keeping. Back in 2017, only 3 out of 10 substance abuse treatment centers in the U.S. relied solely on electronic methods for health record storage. The continued use of paper records creates documentation gaps and makes spotting regional trends a daunting task. Recovery Center CRM steps in to solve this by centralizing patient information - everything from initial contact and treatment history to medical records and demographics - into complete profiles. The system integrates seamlessly with EMRs and call tracking tools, capturing the entire patient journey. This level of detail enables the platform to generate regional insights that support targeted recovery efforts.
The platform goes further by organizing data into categories like age, race, gender, and veteran status. Breaking down these metrics helps uncover disparities in treatment access within specific communities. For instance, Washington State's Health Care Authority leveraged this approach to evaluate opioid use disorder treatments. According to State Opioid Coordinator Kris Shera, their analysis revealed significant gaps in treatment access among Tribal communities, leading the state to allocate direct funding and opioid settlement distributions to these groups.
Recovery Center CRM Features for Regional Analysis
Recovery Center CRM is packed with tools designed to address regional challenges and enhance recovery outcomes through solid, data-driven strategies.
- The Intake & Referral Hub simplifies the referral process from courts and public defenders to accredited treatment programs. It also tracks compliance with court orders and monitors time-to-care metrics.
-
The State-Level Impact Analytics feature compiles large-scale data to evaluate how public funding impacts care across different regions. For example, Indiana's Division of Mental Health and Addiction used this feature to guide decisions that led to the establishment of nine new opioid treatment programs since 2016. The goal? Ensuring that every resident is within an hour’s drive of treatment. Rebecca Buhner, Deputy Director, explained:
"Governor [Eric] Holcomb wanted us to make sure that every Hoosier had access to treatment within an hour's drive, so that's been our goal and our mission".
- The Recovery Housing & Operations suite keeps tabs on bed availability, resident curfews, drug screening results, and housing stability across statewide networks.
Maintaining Compliance and Secure Data Sharing
Sharing regional data across agencies comes with its own set of challenges, especially around security. Recovery Center CRM ensures compliance with HIPAA and SOC 2 Type II standards, utilizing encrypted FHIR (Fast Healthcare Interoperability Resources), Multi-Factor Authentication (MFA), and immutable audit logs in WORM format, which are retained for at least six years. These measures are vital, especially as healthcare hacking incidents have surged by 256% over five years in organizations lacking SOC 2 controls.
The platform also supports controlled data sharing between agencies - like courts, health departments, and housing providers - by managing access at the data-element level. This ensures sensitive information isn't all stored in one vulnerable location. A great example of this approach is Fairfax County, Virginia’s Opioid Policy & Data Framework project, which ran from 2019 to 2022. An advisory group of legal and IT experts developed an Enterprise Memorandum of Understanding to enable eight county entities to share electronic data securely. The system required explicit consent for sharing sensitive substance use treatment data, while other information could be accessed in real time for client interactions.
This secure and integrated system ensures recovery programs are tailored to meet the specific needs of different regions effectively.
sbb-itb-ce23a48
Designing Recovery Programs Based on Regional Data
Adapting Programs to Regional Needs
Regional data plays a crucial role in identifying treatment gaps and understanding which communities need specialized attention. Take Indiana, for instance. The Division of Mental Health and Addiction used a combination of provider availability data and driving distance analysis to pinpoint areas lacking adequate care. Rebecca Buhner, Deputy Director, described the state's commitment:
"Governor [Eric] Holcomb wanted us to make sure that every Hoosier had access to treatment within an hour's drive, so that's been our goal and our mission".
Since 2016, Indiana has established nine new OTPs (opioid treatment programs) and introduced mobile medication units to ensure methadone dosing reaches even the most remote areas.
Breaking data down by factors like race, ethnicity, pregnancy, and veteran status uncovers disparities that might otherwise go unnoticed. This approach allows for targeted funding of critical programs, such as those addressing neonatal abstinence syndrome or supporting Tribal communities. These efforts lay the groundwork for advanced analytics to refine and improve recovery strategies.
Using Analytics to Improve Recovery Outcomes
Analytics take regional insights a step further, helping to allocate resources wisely and hold providers accountable. Louisiana offers a strong example: its Office of Behavioral Health used data from Medicaid-managed care organizations to analyze treatment engagement. Initially, the state ranked below the 50th percentile. However, between 2021 and 2023, a performance improvement project provided feedback to these organizations and tackled regional barriers. The result? Louisiana climbed to the 90th percentile for treatment initiation and the 75th percentile for engagement.
Recovery Center CRM's State-Level Impact Analytics feature gathers large-scale data to show how public funding influences care across regions. It even ranks local programs in real time. Douglas Huntsinger, Indiana’s Executive Director for Drug Prevention, Treatment, and Enforcement, emphasized the impact of meaningful programs:
"That data was able to tell us that if you have a real program, it drastically will change your results".
This kind of analysis helps states identify high-performing models and replicate their success across other regions.
Reducing Administrative Work Through Automation
Efficient recovery management isn’t just about designing programs and analyzing data - it also requires cutting down on administrative burdens. Manual data exchanges between agencies can eat into time that could be spent on patient care. Recovery Center CRM addresses this with automated workflows, allowing secure, role-based data sharing across agencies. This eliminates the need for manual requests and ensures real-time access to crucial information during client interactions. The platform also handles routine tasks like sending appointment reminders, tracking compliance, and updating documentation.
Fairfax County, Virginia, demonstrated the value of automation through its Opioid Policy & Data Framework project (2020–2023). The county developed a secure software solution that enabled staff from mental health services, jails, and social services to access selected data from other agencies when working with clients. The system adhered to strict consent requirements for sensitive substance use data while still providing real-time information during client interactions.
Conclusion: Improving Recovery Through Regional Data
Regional data has proven its ability to transform recovery efforts by addressing the unique needs of specific communities. For example, Louisiana's use of performance data helped the state climb from below the 50th percentile to the 90th percentile in treatment initiation. Similarly, Indiana's decision to add nine new opioid treatment programs based on driving distance analysis has had a measurable, life-saving impact.
The real strength of these efforts comes from pairing data collection with actionable tools. Platforms like Recovery Center CRM play a key role by centralizing patient information, automating workflows, and providing State-Level Impact Analytics to track how public funding translates into care. With real-time analytics, this system identifies treatment gaps, monitors demographic outcomes, and optimizes resource allocation - all while adhering to strict HIPAA and SOC 2 compliance standards. This blend of data and actionable insights creates a foundation for meaningful improvements.
Data alone doesn't drive change - action does. Ohio's 41% drop in opioid doses between 2012 and 2018 happened because the state acted on prescription monitoring data to establish specific prescribing limits. Similarly, Virginia's Addiction and Recovery Treatment Services (ARTS) program achieved a 32% reduction in opioid-related emergency department visits in its second year by aligning services with ASAM criteria. These examples highlight the transformative potential of using regional insights to shape recovery strategies.
Moving forward, breaking down barriers between healthcare providers, justice systems, and community organizations will be essential. Automated systems enable seamless data sharing, cutting down on manual tasks and delivering critical information to decision-makers in real time. This reduces administrative workloads, allowing recovery centers to focus more on patient care - exactly what's needed to improve long-term outcomes for diverse communities.
FAQs
How does using regional data improve outcomes in addiction recovery?
Regional data plays a crucial role in improving addiction recovery outcomes by shedding light on the specific challenges and needs of individual communities. With this information, recovery programs can develop strategies that are tailored to the unique circumstances of a region. For example, it helps pinpoint areas where resources are scarce, like rural regions with limited access to treatment facilities. By examining local trends - such as socioeconomic conditions or patterns of drug use - recovery efforts can become more focused and impactful.
This data also fosters collaboration between key sectors like healthcare, criminal justice, and social services. Together, these groups can create comprehensive recovery programs designed to meet the needs of a specific community. Tools like Recovery Center CRM simplify this process by centralizing and analyzing data, making it easier to track outcomes over time, address service gaps, and adjust programs to better fit local demands. A data-driven approach like this not only improves treatment success but also promotes fair access to recovery resources.
What obstacles do rural communities face in accessing addiction treatment?
Rural communities face tough challenges when it comes to accessing addiction treatment. Many areas simply don’t have enough healthcare resources or treatment facilities. For example, providers who can prescribe medication-assisted treatments (MAT) like buprenorphine - vital for treating opioid use disorder (OUD) - are often in short supply. On top of that, geographic isolation and transportation issues make it even harder for people to reach the care they need.
Another barrier is how rural residents often enter treatment. Many end up in programs through court orders or law enforcement, which points to a lack of accessible outpatient services. Add to this the workforce shortages, economic struggles, and stigma surrounding addiction, and recovery becomes an uphill battle for many.
To tackle these challenges, solutions like telemedicine and community-based initiatives are being explored. These approaches aim to bridge the gap and bring much-needed care to rural areas.
How does technology improve the use of regional data in addiction recovery programs?
Technology plays a key role in making regional data more accessible and actionable for addiction recovery programs. Tools like Recovery Center CRM simplify the process by helping recovery centers track individual progress, monitor demographic trends, and evaluate long-term outcomes - all while adhering to privacy regulations such as HIPAA. By centralizing records and automating routine tasks, these platforms improve both data accuracy and operational efficiency.
On top of that, technology bridges data from a variety of sources, including overdose statistics, treatment histories, and social factors influencing health. This broader perspective helps policymakers and providers pinpoint underserved communities, identify resource gaps, and create tailored recovery programs that address specific local needs. Essentially, technology lays the groundwork for recovery efforts that are guided by data and backed by evidence.

