Top Metrics for Demographic-Based Recovery Analysis
Recovery programs often fail when they ignore the unique needs of different groups. Age, gender, race, and socioeconomic factors all influence recovery outcomes. For example:
- Age: Adolescents (97.5%) and adults (94.7%) with substance use disorders often don't seek treatment because they don't believe they need it. Young adults (18–25) face the highest rates of mental illness and substance use, while older adults (50+) have lower treatment rates.
- Gender: Men and women experience substance use differently. Women face higher rates of co-occurring mental health issues, while treatment barriers often vary by gender.
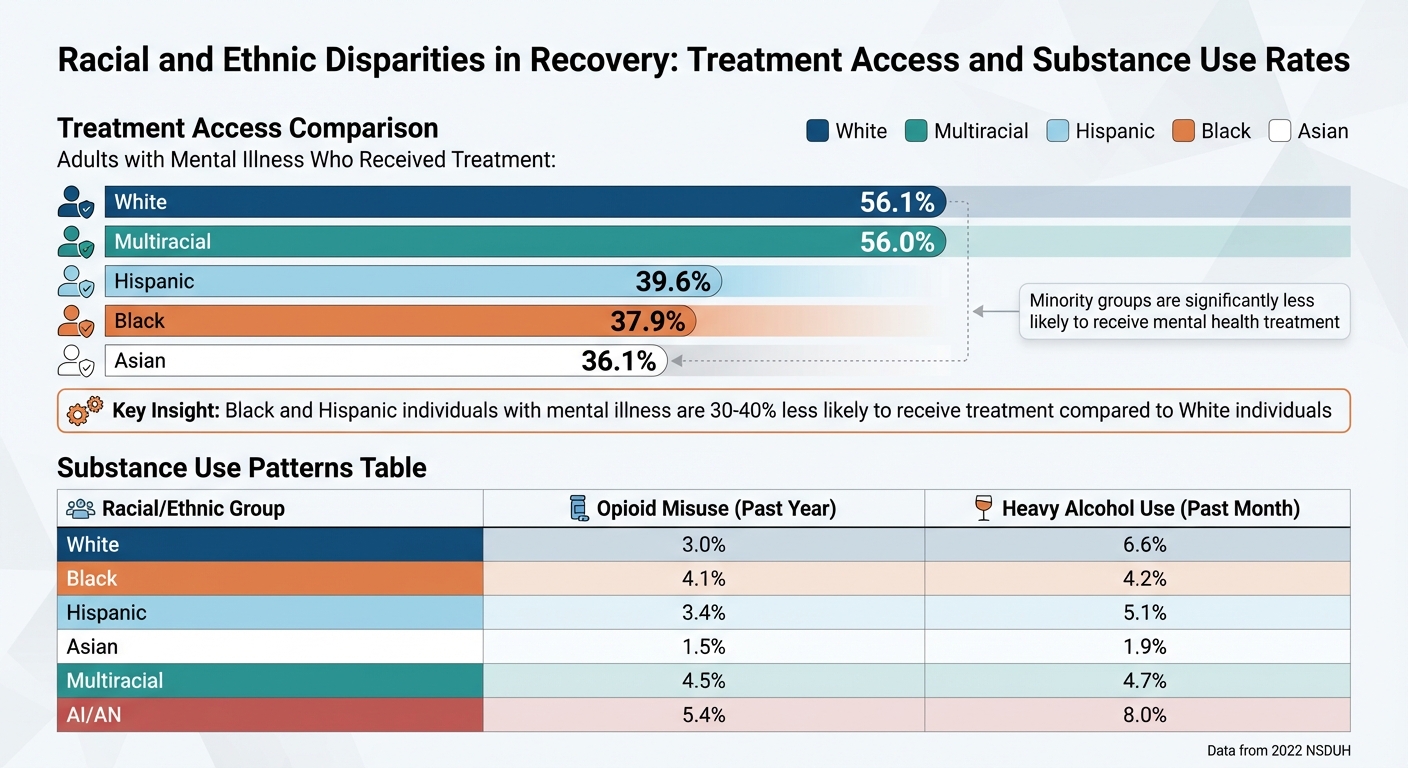
- Race/Ethnicity: Minority groups face lower access to mental health and substance use treatments compared to White individuals. For instance, Black (37.9%) and Hispanic (39.6%) adults with mental illness are less likely to get treatment than White adults (56.1%).
- Socioeconomic Factors: Financial stress and education levels impact access and retention in recovery programs. Low-income individuals with substance use disorders are less likely to complete treatment due to costs and other barriers.
Key takeaway: Tailored recovery efforts are essential. Tools like Recovery Center CRM help track demographic data, identify gaps, and improve outcomes by focusing on the specific needs of individuals and communities.
Age-Based Recovery Metrics
Age plays a significant role in shaping substance preferences and the challenges faced during treatment. For instance, a 16-year-old struggling with vaping encounters vastly different obstacles compared to a 60-year-old who has smoked for decades. To better understand these differences, national recovery data often categorizes populations into three main groups: adolescents (12–17), young adults (18–25), and adults (26 or older). When it comes to mental health and serious mental illness, the 26+ group is sometimes further divided into 26–49 and 50 or older, as treatment rates tend to decline in older populations.
In 2024, 71.5% of adolescents using nicotine products were vaping, while only 18.0% of adults aged 26 or older engaged in vaping. On the other hand, 63.3% of cigarette smokers aged 26 or older are daily smokers (21.6 million people), compared to just 19.5% of smokers aged 18 to 25. These differences highlight the importance of tailoring interventions to the unique needs of each age group.
Treatment Access Rates by Age Group
One of the biggest barriers to recovery is the belief that treatment isn’t necessary. Among adolescents (12–17) with substance use disorders (SUDs), 97.5% did not seek treatment because they didn’t think they needed it, a figure slightly higher than the 94.7% of adults (18+) who felt the same way. Active treatment-seeking is rare across all age groups, with only 0.5% of adolescents and 0.8% of adults with SUDs pursuing care.
Young adults aged 18–25 face particularly steep challenges. In 2022, 48.8% of individuals in this age group had either any mental illness (AMI) or an SUD, a rate significantly higher than the 21.5% seen in adults aged 50 or older. This underscores the need for recovery programs targeting young adults to include robust mental health support alongside substance use treatment. Meanwhile, adults aged 50 or older are less likely to receive mental health treatment (18.0%) compared to young adults (26.7%) or those aged 26–49 (24.5%).
Abstinence Duration and Relapse Patterns by Age
Between 2021 and 2024, certain positive trends emerged. Binge drinking rates dropped for young adults (from 30.0% to 26.7%) and adults aged 26+ (from 22.5% to 20.8%), while remaining steady for adolescents at 3.5%. Tobacco use also saw significant declines across all age groups, with the 26+ age group experiencing a decrease from 22.5% to 18.7%.
Recovery remains a realistic goal for many. Among adults who acknowledged having a substance use problem, 71.0% (approximately 21.3 million people) consider themselves to be in recovery or to have recovered. By examining which age groups maintain longer periods of abstinence and identifying those prone to higher relapse rates, recovery programs can allocate resources more effectively. Tools like Recovery Center CRM help by tracking demographic details alongside recovery progress, uncovering patterns that might otherwise go unnoticed in broader datasets. These insights into age-specific recovery trends pave the way for more targeted and effective interventions.
sbb-itb-ce23a48
Gender-Based Recovery Metrics
Gender significantly influences the development of substance use issues, access to treatment, and the likelihood of completing recovery programs. National guidelines reflect these differences. For instance, binge drinking is defined as five or more drinks for males and four or more drinks for females on the same occasion. These distinctions stem from biological differences in how alcohol is metabolized, making gender-specific thresholds critical for accurate screening and tailored interventions. Understanding these foundational differences helps in exploring substance use trends and treatment outcomes across genders.
Substance Use Disorder Rates by Gender
Patterns of substance use often differ between genders, and recognizing these differences is key to designing effective interventions. In 2022, 48.7 million people aged 12 or older (17.3% of the population) were reported to have a substance use disorder. Among them, 29.5 million faced alcohol use disorders, 27.2 million dealt with drug use disorders, and 8.0 million struggled with both. Federal reports now consolidate data to examine disparities by sex, race, and age, acknowledging that these factors heavily influence recovery outcomes.
Failing to account for gender-specific needs may lead to misdiagnosing treatment requirements or applying generalized solutions that overlook the unique challenges faced by men and women.
Treatment Access and Completion Rates by Gender
Gender differences extend beyond substance use patterns, shaping both access to treatment and recovery success. Barriers to treatment vary between genders, requiring programs to adopt tailored outreach strategies. These barriers, while universal in some respects, often manifest differently for men and women. Effective recovery programs must address these challenges through education and outreach efforts that resonate with each gender's specific concerns.
Gender-specific support is vital because treatment completion rates and recovery paths often diverge between men and women. Policies that explicitly protect against discrimination based on gender, pregnancy, sexual orientation, or identity are crucial for ensuring fair access to treatment. As outlined by SAMHSA, the agency adheres to federal laws prohibiting discrimination based on "race, color, national origin, age, disability, religion, or sex (including pregnancy, sexual orientation, and gender identity)".
Tools like advanced addiction treatment CRM systems can help track these gender-based metrics, allowing programs to refine their approaches and address disparities effectively. By focusing on these nuanced differences, recovery programs can create more equitable and impactful outcomes.
Racial and Ethnic Disparities in Recovery
Mental Health Treatment Access Disparities by Race and Ethnicity
Race and ethnicity play a significant role in shaping the prevalence of substance use disorders (SUD) and access to treatment. A deeper understanding of these disparities is essential for creating recovery strategies that are truly effective for diverse populations. To capture the complexities of these differences, researchers often rely on pooled data, such as five-year averages, to ensure sample sizes are large enough to analyze groups like Hispanic/Latino, Black, Asian, and Native American communities. Without this detailed approach, recovery programs risk implementing generic solutions that overlook the unique challenges faced by specific populations. The following data highlights how racial and ethnic factors influence recovery outcomes.
Treatment Access Barriers for Minority Groups
Access to treatment for SUD and mental health issues can vary greatly depending on race and ethnicity, even when prevalence rates are similar. For example, among adults with any mental illness (AMI), Asian (36.1%), Black (37.9%), and Hispanic (39.6%) individuals are far less likely to receive mental health treatment compared to White (56.1%) or Multiracial (56.0%) individuals. These disparities point to systemic barriers, such as unmet needs and inconsistent engagement, that disproportionately affect minority groups. Studies have also shown that geographic factors play a role. In one multi-state study, Black clients in New York and American Indian clients in Washington were significantly less likely to engage in treatment compared to White clients.
Mapping the locations of buprenorphine prescribers and methadone clinics against neighborhood demographics reveals clear "treatment deserts" in areas where minority communities experience high SUD rates but have limited access to care. To address these gaps, recovery programs should monitor provider distribution and consider the travel times required to reach facilities.
Substance Use Disorder Rates by Race and Ethnicity
In addition to access barriers, variations in substance use rates across racial and ethnic groups further highlight the need for tailored interventions. For instance, past-year opioid misuse (including heroin and prescription pain relievers) is more common among Multiracial (4.5%), Black (4.1%), and Hispanic (3.4%) individuals compared to Asian individuals (1.5%). Similarly, patterns of heavy alcohol use differ by group, with White individuals (6.6%) showing higher rates than Hispanic (5.1%), Black (4.2%), or Asian (1.9%) individuals in 2022.
| Racial/Ethnic Group | Opioid Misuse (Past Year) | Heavy Alcohol Use (Past Month) | Received MH Treatment (if AMI present) |
|---|---|---|---|
| White | 3.0% | 6.6% | 56.1% |
| Black | 4.1% | 4.2% | 37.9% |
| Hispanic | 3.4% | 5.1% | 39.6% |
| Asian | 1.5% | 1.9% | 36.1% |
| Multiracial | 4.5% | 4.7% | 56.0% |
| AI/AN | 5.4% | 8.0% | N/A (Low Precision) |
Note: AI/AN = American Indian or Alaska Native; data from 2022 NSDUH.
Tools like Recovery Center CRM can help track these metrics, identify underserved areas, and improve outreach efforts to ensure equitable access to treatment. Just as age and gender data inform recovery strategies, racial and ethnic insights can guide programs to close treatment gaps and provide more effective support.
Socioeconomic Factors in Recovery
Socioeconomic factors play a powerful role in shaping recovery outcomes, going beyond age, gender, and race. Elements like income, education, and employment can determine whether someone enters treatment and how well they sustain long-term recovery. Financial stress, for example, can derail recovery efforts by adding worries about costs. Those with lower incomes and substance use disorders face some of the highest mortality risks but are also the least likely to stick with treatment programs consistently. Recognizing these patterns allows recovery programs to pinpoint at-risk groups and create strategies that address the real challenges people face in accessing and completing treatment. The impact of financial barriers is particularly evident in treatment engagement statistics.
Income Level and Treatment Completion Rates
For low-income populations, financial hurdles can make it incredibly difficult to engage with treatment programs. A study of 159,016 adult Medicaid recipients showed alcohol treatment engagement rates ranging from 0% to 0.4%, while opioid treatment engagement varied between 41.5% and 61.4%. These numbers highlight the challenges Medicaid-managed care plans face in connecting financially vulnerable individuals with the care they need.
Financial insecurity doesn’t just affect access - it also impacts retention and completion. Complex billing systems and unexpected costs often lead to higher dropout rates. Simplifying billing processes and aiming for at least 85% patient satisfaction in financial clarity can ease these stresses and boost treatment retention. Stable employment and secure housing, meanwhile, are not just contributing factors to recovery - they’re also key indicators of successful treatment outcomes.
But financial barriers are only part of the story. Differences in education levels also play a critical role in recovery outcomes.
Education Level and Recovery Outcomes
Education shapes how well individuals can navigate the healthcare system and engage with recovery resources. People with higher levels of education often have better health literacy, which makes it easier for them to understand and act on complex treatment information. This connection between education and health outcomes begins long before clinical interventions, as higher education levels often lead to better health literacy and fewer complications down the road.
"Education level... will also protect against certain healthcare [challenges]." – Healthcare Professional, PMC Qualitative Study
In addition to improving access to treatment information, higher education could help reduce the 90% of healthcare spending that goes toward chronic and mental health conditions by preventing complications. On the flip side, individuals with lower levels of education are more likely to face poor health outcomes, emphasizing the need for outreach efforts focused on education and simplified communication strategies to make recovery more accessible.
Court-Ordered Recovery Metrics
Court-ordered recovery metrics shine a spotlight on the unique challenges faced by different demographic groups during their recovery journeys. The justice system often serves as a critical gateway to treatment, especially for individuals who might not seek help on their own. In fact, court-mandated programs account for about 36% of all substance abuse treatment admissions and a striking 57% of marijuana-related admissions. By tracking these metrics, we gain valuable insights into the speed of treatment initiation, its duration, and the specific hurdles faced by various populations. These findings are vital for improving recovery outcomes and promoting fairness in access to care.
Time-to-Care for Court-Ordered Referrals
The time it takes to move from a court referral to the start of treatment can significantly influence recovery success. For example, a critical benchmark for opioid use disorder (OUD) is starting treatment within 14 days of diagnosis. Across 39 states, 55% of Medicaid participants hit this mark, but only 39% received follow-up care within 34 days. This gap in ongoing care highlights a concerning trend: many individuals are not receiving the continuous support necessary to maintain recovery.
Geographic disparities further complicate access. In some rural counties in Pennsylvania, fewer than 20% of Medicaid participants with OUD received a diagnosis in primary care settings, even with regular doctor visits. Dr. Katherine Marks, who leads the Kentucky Opioid Response Effort, underscores the importance of data-driven approaches:
"You've got to follow the data to know where you've been and where you need to go, right? Or it's not just a lost opportunity, it's lost lives when we're not data-driven".
Beyond initial access, retention in treatment plays a crucial role. Evidence shows that treatment lasting at least 90 days leads to significant reductions in drug use and criminal behavior. Common metrics for measuring success include 90-day engagement and 6-month (180-day) continuity of pharmacotherapy. To ensure accuracy, programs increasingly rely on documented drug and alcohol tests instead of self-reported data, allowing them to identify when participants are struggling.
These access and retention challenges provide important context for understanding compliance differences among demographic groups.
Compliance Rates by Demographics
When it comes to compliance, court-ordered mandates often act as strong motivators. Individuals in mandated programs are over 10 times more likely to complete intensive outpatient treatment than those who enter voluntarily (OR = 10.9). However, compliance rates vary widely across demographic groups, revealing disparities that recovery programs must address.
Age is a key factor, with younger participants often showing lower completion rates compared to older individuals. Socioeconomic status also influences outcomes. Those with severe employment challenges or lower levels of education are more likely to drop out of treatment. For instance, individuals without a high school diploma are nearly 6 times more likely than college graduates to enter substance abuse programs, largely due to referrals from the criminal justice system.
Gender adds another layer of complexity. Women in the justice system face unique challenges, including higher rates of co-occurring mental health conditions (66% compared to 37% for men). Many women also fail initial employment-integrated recovery screenings because of unstable psychiatric conditions, and fears of losing child custody further complicate their recovery journeys.
To address these disparities, recovery programs must break down metrics by race, ethnicity, age, gender, and geography. Additionally, identifying reasons for non-completion - such as criminal involvement, missed appointments, relocation, or even death - can help pinpoint where interventions are most needed.
Using Recovery Center CRM for Demographic Analysis
Tracking demographic metrics effectively is no small feat, especially when relying on spreadsheets and manual reporting. Recovery Center CRM simplifies this process by centralizing documentation while adhering to HIPAA and SOC 2 compliance standards. This ensures that state health departments, justice systems, and recovery housing providers can securely share data using role-based permissions. With everything in one place, programs can dive into tailored analytics that span multiple dimensions of their initiatives.
Customizable Demographic Profiles and Reports
Recovery Center CRM makes it easier to analyze data by breaking it down into categories like race, ethnicity, age, gender, and insurance status. This granular approach helps uncover health disparities that might otherwise remain hidden in aggregated numbers. By filling this reporting gap, the platform provides insights that many states currently lack.
The flexibility of customizable fields means recovery centers can focus on the metrics that matter most to their communities. For example, they can track whether specific age groups are starting treatment within the critical 14-day window after diagnosis or identify if gender disparities exist in treatment completion rates. These insights are more than just numbers - they guide targeted interventions and resource allocation. Identifying disparities helps programs address barriers head-on, improving outcomes for underserved populations.
State-Level Impact Analytics
State health departments rely on aggregated data to showcase the impact of public funding and ensure compliance with federal regulations. Recovery Center CRM supports this need by tracking mandatory metrics tied to programs like the Medicaid 1115 SUD waiver, such as pharmacotherapy use and follow-up care after emergency department visits. These metrics address long-standing gaps in monitoring and reporting.
The platform uses a cascade of care framework to map the entire journey from diagnosis to long-term recovery. This approach pinpoints where gaps exist in the care continuum. Combined with demographic data, these analytics provide a clearer picture of recovery outcomes, helping policymakers direct interventions and resources to where they’re needed most. For instance, rural areas with limited provider coverage can be prioritized for additional support.
Recovery Housing and Operational Metrics
Operational data is just as crucial as state-level oversight, especially for improving program performance on the ground. For recovery housing networks, Recovery Center CRM tracks bed availability, resident curfews, drug screening results, and housing stability across entire state systems. Housing stability metrics - measured at 90 days, six months, and beyond - serve as key indicators of successful reintegration. Programs can also break down these metrics by demographic factors, identifying which groups may need extra support to maintain stable housing during recovery.
The platform’s Justice-to-Community Journey module plays a vital role in managing transitions for individuals moving from incarceration back into their communities. By ensuring medical records and recovery plans follow individuals across institutional boundaries, this module facilitates "warm handoffs". Additionally, it tracks time-to-care for court-ordered referrals alongside demographic data, revealing delays that may disproportionately impact specific populations. These insights can help programs improve access and equity in treatment for justice-involved individuals.
Conclusion
Tracking metrics based on demographics isn’t just about crunching numbers - it’s about saving lives and creating fair opportunities for recovery. When programs break down data by factors like age, gender, race, and socioeconomic status, they uncover disparities that often stay hidden in broad, aggregated reports. These details highlight which communities face the toughest challenges in accessing treatment and show exactly where resources need to be directed. This targeted, data-focused approach forms the backbone of the solutions provided by Recovery Center CRM.
To put things in perspective, only 12% of individuals with Opioid Use Disorder received necessary medications in 2020. That statistic represents countless people who missed out on the help they desperately needed.
Recovery Center CRM steps in by centralizing demographic tracking, making it easier to identify and address gaps in treatment. Its customizable features allow programs to monitor key metrics, whether that’s tracking whether patients start treatment within 14 days or spotting disparities in completion rates between genders. By combining operational data with demographic insights, as discussed earlier, Recovery Center CRM equips recovery programs to take action where it matters most. It provides a clear view of who is being served - and who might be slipping through the cracks.
By using this kind of integrated analysis, recovery programs can make smarter decisions. The cascade of care framework, for example, pinpoints exactly where different demographic groups tend to drop out of treatment. This insight helps programs allocate resources more effectively. For state health departments managing public funding, this level of transparency not only builds trust but also shows lawmakers and federal grant administrators the real impact of their investments. At the same time, it ensures that interventions are tailored to the specific challenges faced by each community.
FAQs
How do recovery trends differ by age, and why does it matter for treatment strategies?
Age-related recovery patterns are key to crafting treatment strategies that address the specific needs of different age groups. For older adults, recovery often means managing overlapping health issues like chronic diseases or cognitive impairments, which can heavily influence their progress. On top of that, the increasing number of older adults dealing with substance use problems has highlighted the need for specialized approaches. These might include adjusted counseling techniques, careful medication management, and stronger social support networks.
By recognizing these patterns, recovery programs can develop strategies tailored to each age group, boosting the chances of long-term success. Tools like Recovery Center CRM play a vital role in this process, helping providers gather demographic insights, track outcomes, and design programs that align with the unique needs of various age groups. This ensures that treatment remains effective and responsive to the people it aims to help.
What challenges do minority groups face in accessing treatment programs?
Minority groups often face distinct hurdles when trying to access treatment programs, many of which stem from systemic and social inequalities. For instance, economic challenges, such as poverty, can make healthcare unaffordable, while limited access to healthcare services creates significant delays or even prevents individuals from receiving the care they need. On top of this, discrimination and stigma tied to cultural norms can discourage people from seeking help altogether.
Another major issue lies in the lack of diverse and culturally aware staff in many programs. Without professionals who understand and respect different cultural perspectives or who can provide services in multiple languages, it becomes even more difficult to serve diverse communities effectively. Tackling these issues calls for a deeper commitment to community involvement, tailoring interventions to reflect cultural needs, and addressing the social and economic inequalities that disproportionately impact minority populations.
How do socioeconomic factors impact the success of recovery programs?
Socioeconomic factors are deeply intertwined with the effectiveness of recovery programs, shaping access to resources, stability, and support networks. Elements such as income, housing stability, employment opportunities, and social connections can either bolster or undermine recovery efforts. For example, individuals struggling with financial hardship or unstable housing often face a greater risk of relapse. A safe and secure living environment, coupled with financial stability, is fundamental for sustaining long-term recovery.
Inequalities in access to healthcare and treatment services, often rooted in socioeconomic disparities, can further limit participation in recovery programs and diminish their impact. Leveraging demographic and socioeconomic data allows recovery programs to adapt their services, addressing these barriers and ensuring care is both equitable and responsive. Tackling these challenges is essential for building effective recovery plans and supporting enduring success.

