How Relapse Risk Monitoring Improves Recovery Outcomes
Relapse risk monitoring helps individuals in recovery by identifying early warning signs and providing opportunities for timely intervention. This approach treats addiction as a chronic condition, similar to diabetes or hypertension, requiring continuous care and tracking. Key insights include:
- Relapse is a gradual process: Emotional, mental, and physical changes often signal risks before a relapse occurs.
- Statistics highlight the need for monitoring: About 50% of individuals relapse within 12 weeks after inpatient programs, emphasizing the importance of ongoing support.
- Personalized prevention plans: Tailored strategies address specific triggers and coping mechanisms.
- The role of technology: Tools like apps, wearable devices, and centralized systems track risk factors (e.g., cravings, depression) and protective behaviors (e.g., support group attendance).
- Data-driven adjustments: Monitoring progress allows for real-time treatment changes, improving engagement and outcomes.
Relapse Prevention Awareness: Addiction Recovery Counseling Tools
sbb-itb-ce23a48
What Causes Relapse and How to Spot Warning Signs
Three-Stage Relapse Process and Warning Signs in Addiction Recovery
Risk Factors That Lead to Relapse
Negative emotions play a major role in more than half of relapse episodes. Feelings like anger, anxiety, depression, frustration, and even boredom significantly increase the risk of slipping back into old habits. Interpersonal conflicts - such as arguments with family, friends, or coworkers - are another common trigger, while social pressure accounts for over 20% of relapses.
Lifestyle imbalances also contribute. When external pressures outweigh personal satisfaction, stress builds, leading to small but risky choices. These Apparently Irrelevant Decisions (AIDs) - like buying alcohol for a party or taking a route that passes a tempting spot - might seem harmless but can inch someone closer to relapse.
On a biological level, changes in brain chemistry also play a part. Higher basal ACTH levels, altered cortisol responses, and increased BDNF levels have been linked to shorter times before relapse. These physiological markers highlight the measurable impact addiction has on the brain.
Fortunately, these risks often show up as noticeable behaviors, offering clues that a relapse could be on the horizon.
Warning Signs That Relapse May Be Coming
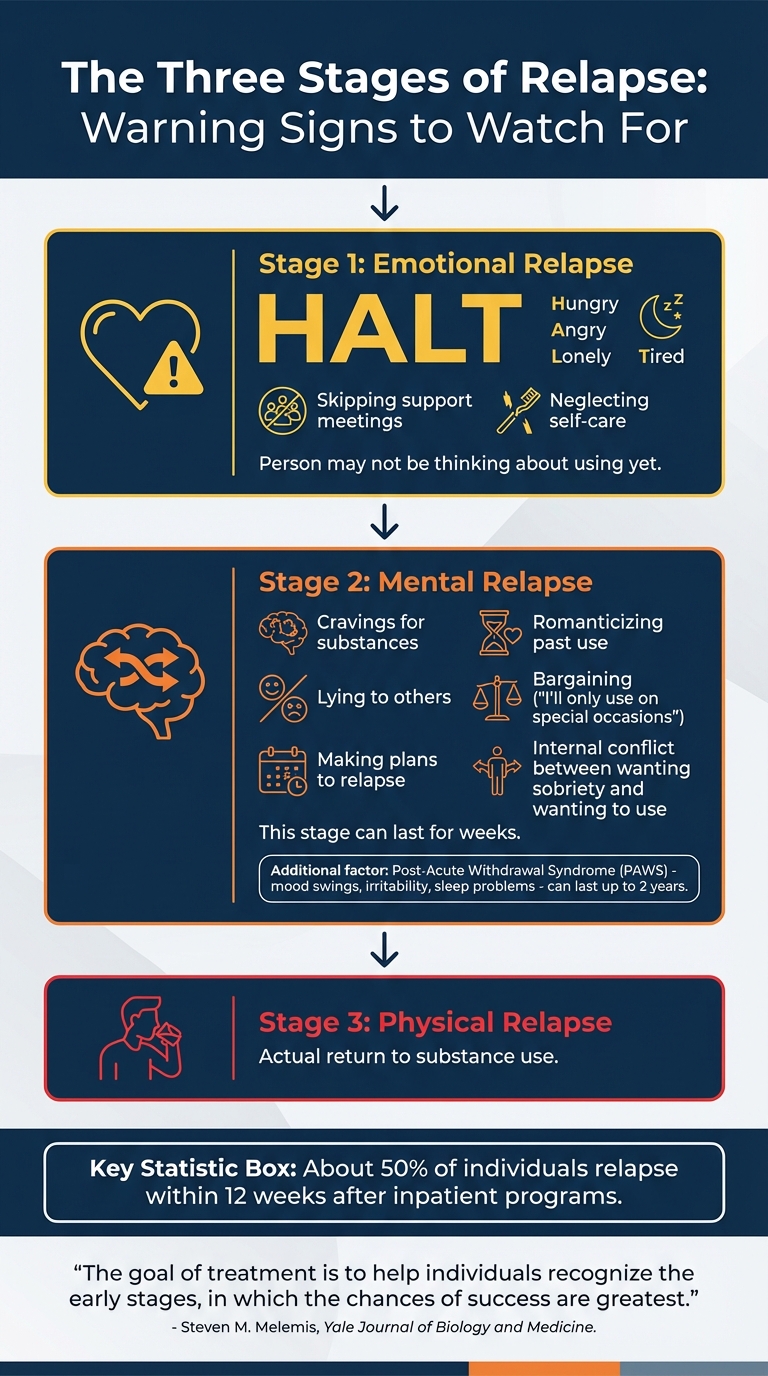
The acronym HALT - Hungry, Angry, Lonely, Tired - points to key signs of poor self-care and emotional relapse. If someone starts isolating themselves, skipping support meetings, suppressing emotions, or neglecting basic needs like eating or sleeping, they may already be in the emotional stage of relapse, even if using hasn't crossed their mind.
"The goal of treatment is to help individuals recognize the early stages, in which the chances of success are greatest." - Steven M. Melemis, Yale Journal of Biology and Medicine
Mental relapse comes with clearer warning signs. These include cravings, romanticizing past use, lying, bargaining ("I'll only use on special occasions"), and even making plans to relapse. This internal tug-of-war - wanting to stay sober but also wanting to use - can go on for weeks. Post-Acute Withdrawal Syndrome (PAWS), which includes mood swings, irritability, and trouble sleeping, often adds to the challenge. These symptoms can last up to two years, leaving individuals feeling stuck and frustrated, which can push them toward relapse.
How to Set Up a Relapse Monitoring System
Setting up a relapse monitoring system involves three essential steps: crafting personalized prevention plans, scheduling regular check-ins, and using technology to centralize data. A well-structured system like this can significantly improve recovery outcomes.
Create Individual Prevention Plans
Recovery looks different for everyone, so prevention plans should be tailored to each individual’s specific triggers and strengths. Start by identifying both internal triggers - like boredom, anger, or stress - and external ones, such as certain places, people, or social situations.
Once triggers are identified, pair each one with a coping strategy. For example, if loneliness is a trigger, the plan might include calling a sponsor or attending a peer support meeting. For cravings, techniques like "urge surfing" can be helpful - this involves visualizing cravings as waves that rise and eventually subside. Incorporate tools like the HALT check (Hungry, Angry, Lonely, Tired) into daily routines to catch vulnerabilities before they escalate.
"A relapse prevention plan should be a living document that changes and grows over time." - Allison Ward, Center for Practice Transformation
Role-playing these strategies can help build confidence and uncover potential challenges. Sharing the finalized plan with the individual’s support network - whether that’s family, sponsors, or healthcare providers - ensures everyone is on the same page about warning signs and how to intervene. These personalized plans also lay the foundation for meaningful follow-ups during check-ins.
Schedule Regular Check-Ins and Track Data
After creating prevention plans, consistent follow-up is key to catching issues early. Regular check-ins combined with systematic data tracking help monitor progress and identify when adjustments are needed. Tools like PHQ-9 (for depression), GAD-7 (for anxiety), and TAPS (for substance use risk) provide measurable insights over time. These tools allow care providers to gauge whether treatments are effective or need tweaking.
Assign a team member to routinely review patient data, such as attendance and progress metrics, to spot red flags. For example, at UPMC Matilda Theiss Health Center, social workers conducted home visits to re-engage patients who had stopped attending appointments, successfully bringing them back into regular care. This kind of proactive monitoring ensures no one gets overlooked.
Tracking attendance and clinical outcomes is crucial. If someone misses appointments or their PHQ-9 scores worsen, the system should flag them for immediate attention. Research shows that staying engaged in treatment for at least three months is critical for reducing substance use, making this monitoring period especially important.
Use Technology to Track Relapse Risks
Technology can streamline relapse monitoring by centralizing data and making it easier to identify patterns. Platforms like Recovery Center CRM (https://beepurple.com) allow care teams to track treatment progress, set goals, and adjust plans as needed - all in one place. This eliminates inefficiencies caused by scattered spreadsheets or paper files.
Automated alerts are another powerful tool. For instance, if someone misses an appointment or reports high distress during a HALT check-in, the system can notify staff immediately. Community Health Plan of Washington uses a Care Management Tracking System to schedule appointments, track referrals, and monitor progress, ensuring follow-up for at-risk patients.
Remote monitoring tools extend care beyond the clinic. Mobile apps can collect self-reported outcomes, medication adherence data, and daily HALT checks, while wearable devices track metrics like sleep patterns or heart rate. This real-time data allows providers to quickly adjust treatment plans, refine diagnoses, or address struggles with adherence. By integrating these tools, care teams can respond swiftly and effectively to potential setbacks.
"Good Information = Good Outcomes" - Dr. David Miles, PharmD
Digital systems also ensure smooth care transitions by providing instant access to relapse prevention plans, supporting continuity and reducing the risk of relapse during critical moments.
How Monitoring Data Improves Recovery Results
Using data to monitor recovery transforms it from a trial-and-error process into a more focused and effective approach. With data, providers can identify what’s working, pinpoint areas needing improvement, and adapt treatment plans accordingly.
Adjust Treatment Plans Using Monitoring Data
Monitoring data allows for a "treatment to target" approach - similar to how diabetes is managed. For instance, if a patient’s PHQ-9 scores remain elevated or cravings persist, the treatment plan can be adjusted immediately to address these issues.
This approach often follows a stepped-care model, starting with less intensive interventions and escalating as needed based on the data. For example, if a patient’s Progress Assessment (PA) highlights ongoing high-risk situations and low self-efficacy despite outpatient counseling, it may signal the need for more intensive clinical support.
A real-world example of this comes from Chestnut Health Systems, which implemented Recovery Management Checkups (RMC) with 448 adults in Chicago between February and April 2000. Led by Christy K. Scott and Michael L. Dennis, the program used quarterly monitoring and motivational interviewing to address barriers revealed by the data. This approach improved patient engagement and extended treatment durations.
Moreover, data monitoring can uncover external challenges affecting recovery. For instance, if a patient frequently misses appointments, tracking might reveal issues like transportation problems, childcare conflicts, or housing instability. These insights allow providers to adjust care plans to address these barriers rather than assuming the solution is more counseling sessions. In New York State, the LOCADTR 3.0 system linked 80% of individuals from a database of 830,000 assessments to a statewide treatment registry. This system highlighted gaps in service capacity, with clinicians needing to override data-driven recommendations in only 10% of cases.
"If patients are not reaching treatment goals, treatment should be modified - this is often referred to as 'treatment to target.'"
By leveraging data, clinicians can make informed decisions that form the foundation of a proactive, comprehensive recovery plan. This approach not only addresses immediate needs but also supports long-term progress.
Track Progress Over Time
In addition to enabling immediate treatment adjustments, consistent tracking helps solidify recovery progress over time. Regularly measuring progress motivates patients and holds them accountable. For example, when patients see graphs showing improvements in sleep quality, lower anxiety levels, or more days of abstinence, it reinforces the value of their efforts. Tools like NIH PROMIS make this process simple, delivering precise clinical scores in under two minutes with just a few questions.
Progress tracking also helps identify potential gaps in care before they escalate into crises. In a study conducted in October 2020, researchers Kevin G. Lynch and James R. McKay used a 10-item Progress Assessment (PA) to track 158 cocaine-dependent patients over 12 months. By evaluating risk and protective factors every three months, clinicians could predict urine toxicology results and adjust treatment proactively - addressing triggers like depressed mood or low self-efficacy before they led to relapse.
Long-term tracking is especially important since recovery is a gradual process. It often takes three to five years of sustained recovery for relapse risks to significantly decrease. Consistent monitoring enables early re-intervention (ERI), helping identify individuals who may need additional support before a relapse occurs.
"Monitoring symptoms should begin while still in treatment, and then extend into recovery on a regular basis."
- A. Thomas McLellan, Founder of the Treatment Research Institute
Platforms like Recovery Center CRM (https://beepurple.com) simplify this process by centralizing long-term data. These tools provide a clear view of trends across various aspects of recovery, from substance use patterns to social support engagement. This comprehensive perspective ensures that care teams can make well-informed adjustments, based on the full scope of a patient’s progress rather than isolated metrics.
Connect People to Support Networks Using Monitoring Data
Monitoring data doesn’t just track progress - it plays a vital role in identifying when individuals need additional support, helping to prevent relapse. By integrating this data into personalized treatment plans, care providers can strengthen recovery networks and offer timely interventions.
How Peer Support and Community Resources Help
Recovery thrives on a solid support system. Peer support groups like AA, NA, and SMART Recovery offer more than accountability - they create a space where individuals can connect with others who truly understand the recovery journey. These groups bring a level of shared experience and empathy that clinical treatment alone can’t replicate.
Community resources also play a crucial role by addressing practical challenges that could jeopardize recovery. Services such as stable housing, job training, legal aid, and access to primary care provide a safety net for individuals navigating recovery. For example, when monitoring data flags issues like homelessness, providers can step in early, connecting individuals with the necessary resources to address these stressors before they lead to relapse.
"Recovery from problematic substance use is a highly personal journey toward wellness, satisfying relationships, engagement in community, and a sense of meaning and purpose."
The power of monitoring data is backed by research. From February to April 2000, the Haymarket Center in Chicago conducted a Recovery Management Checkup (RMC) study with 448 adults. Participants underwent quarterly assessments, and when the data suggested a need for treatment - such as frequent substance use or withdrawal symptoms - they were connected to a Linkage Manager. These managers used motivational interviewing to help overcome barriers and facilitate treatment reentry. Over 24 months, participants in the RMC group returned to treatment faster and spent more days in treatment compared to those in the control group.
Know When to Add More Support
Monitoring systems act as an early warning system, identifying signs of social isolation or declining engagement. For instance, data can reveal emotional relapse indicators like skipping support meetings, poor sleep or eating habits, or withdrawing from social activities. These are often cues that peer re-engagement or motivational interviewing may be needed.
As isolation deepens, tailored interventions become even more critical. Monitoring also sheds light on environmental risks - such as drug use in the home, a lack of sober friends, or harmful social influences like interpersonal conflict or pressure to use substances. These insights enable providers to determine when stronger community-based support, such as sober living arrangements or increased peer contact, might be necessary.
Platforms like Recovery Center CRM (https://beepurple.com) streamline this process by centralizing data on social support and clinical metrics. These tools flag individuals showing signs of isolation or disengagement, ensuring care teams can act quickly to connect them with the peer support and community resources essential for lasting recovery.
Conclusion
Relapse risk monitoring has the potential to reshape recovery journeys by spotting warning signs before they lead to a return to substance use. Statistics reveal that nearly 50% of alcohol-dependent individuals relapse within just three months of detoxification. By focusing on early emotional and mental signals - like isolation, neglecting self-care, or cravings - monitoring systems create opportunities for timely interventions when they are most effective. These insights pave the way for a proactive, data-informed recovery process.
Long-term recovery often requires ongoing care for 3–5 years, during which regular tracking allows for immediate adjustments to treatment plans. This "treatment-to-target" method ensures that providers can respond quickly when patients struggle to meet their goals. The use of data-driven approaches customizes care to fit each individual’s unique needs.
Technology plays a key role in simplifying this process. Tools like Recovery Center CRM (https://beepurple.com) consolidate critical data on behaviors, social support, and clinical metrics. This centralized system enables providers to act swiftly when signs of disengagement or increased risk emerge.
"The goal of treatment is to help individuals recognize the early stages [of relapse], in which the chances of success are greatest."
- Steven M. Melemis, MD, Ph.D.
Data-driven monitoring doesn't just personalize care - it makes it more effective. Around 60% of people with substance dependence eventually achieve lasting recovery, often after several treatment attempts. By reducing the duration of relapses, strengthening connections to support networks, and adapting treatment in real time, monitoring systems are making a measurable difference - and saving lives.
FAQs
How can technology help monitor and reduce relapse risks during recovery?
Technology is transforming how we monitor relapse risks by introducing real-time tracking and data-driven insights into the recovery process. Tools like AI-powered algorithms, wearable devices, and behavioral analytics can identify early signs of relapse, allowing for timely and effective interventions. These advancements go beyond the scope of traditional methods, enabling recovery programs to offer more tailored and responsive support.
On top of that, digital solutions such as clinician-administered assessments and the use of digital biomarkers make it easier to monitor progress and adapt treatment plans as needed. Platforms like Recovery Center CRM bring these features together, streamlining data collection and providing actionable insights to enhance recovery efforts. By incorporating technology, recovery centers can offer stronger, more personalized support on the journey to long-term wellness.
What are the early signs that someone might relapse?
Relapse often starts with subtle shifts in behavior, emotions, and daily routines - sometimes surfacing weeks or even months before substance use begins again. Early warning signs might include pulling away from support systems like therapy or group meetings, experiencing mood swings, heightened anxiety, or difficulty sleeping. Changes in behavior, such as becoming more defensive, acting impulsively, or retreating into isolation, can also signal trouble.
Stress, feelings of failure, or exposure to environments tied to past substance use can act as emotional triggers, increasing the chance of relapse. Spotting these signs early opens the door for timely intervention and tailored support. Tools like Recovery Center CRM can play a key role by monitoring behavioral and emotional patterns, helping to reduce the risk of relapse.
How do personalized prevention plans support lasting recovery?
Personalized prevention plans are essential for supporting lasting recovery because they focus on each person's specific needs, strengths, and challenges. These plans work by identifying potential relapse risks and setting clear, actionable goals to address them. This approach empowers individuals to better manage triggers and develop healthier coping strategies.
By regularly tracking progress and adjusting strategies when necessary, these plans ensure that recovery efforts stay effective over time. Tools like data-driven platforms allow recovery centers to monitor progress, analyze important metrics, and fine-tune their methods. This not only boosts confidence but also helps lower the risk of relapse and encourages long-term recovery success.