Real-Time Documentation: Solving Data Silos in Recovery
Data silos create major challenges in addiction recovery programs. They lead to fragmented care, missed opportunities for intervention, and inefficiencies that waste staff time. Real-time documentation offers a solution by centralizing and updating client information instantly across teams. This ensures care providers always have access to the latest data, improving decision-making and coordination.
Key Insights:
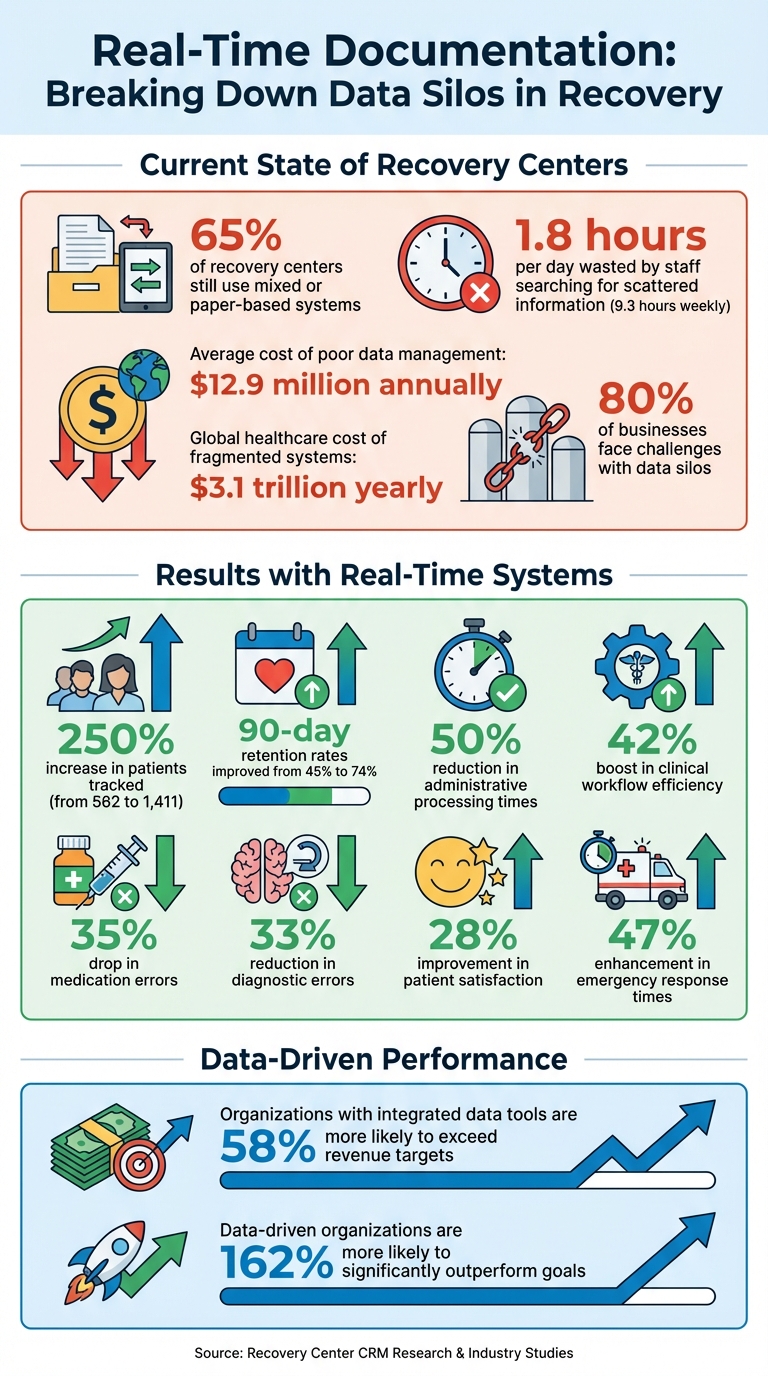
- 65% of recovery centers still use mixed or paper-based systems, creating barriers to care.
- 1.8 hours per day are wasted by staff searching for scattered information.
- Real-time systems unify intake, clinical, and billing data into a single platform, eliminating delays and errors.
- Features like centralized databases, automated workflows, and role-based permissions enhance efficiency and security.
By adopting tools like Recovery Center CRM, recovery programs can streamline operations, improve client outcomes, and ensure compliance with regulations like HIPAA. The result? Faster access to critical information, better care coordination, and more effective recovery support.
Real-Time Documentation Impact on Recovery Centers: Key Statistics
Case Management for a Substance Abuse Treatment Center (FileMaker in Action 006)
How Real-Time Documentation Works in Recovery
Real-time documentation involves recording and updating client information as events occur. For example, when an intake coordinator logs a new biopsychosocial assessment or a counselor updates a treatment plan, that information becomes instantly accessible to all relevant staff. This means case managers, clinical supervisors, and administrative teams are always working with up-to-date data. If a client transitions from an emergency department to a specialized addiction clinic, the receiving team can immediately access the full patient history - no need for phone calls or faxed records.
This approach establishes what experts refer to as a "single source of truth". Instead of different teams maintaining separate records - like spreadsheets, standalone databases, or paper files - everyone works from a unified system. This centralization offers a comprehensive view of each client’s recovery journey, covering everything from housing and employment services to clinical progress. By eliminating delays and confusion, this system lays the groundwork for breaking down data silos.
What Real-Time Documentation Means
In recovery settings, timing is critical. Real-time documentation ensures that vital information is available exactly when it’s needed. For instance, a counselor aware of a client’s recent emergency room visit can address potential relapse triggers during the next session. Similarly, a case manager with updated medication details can better coordinate care with primary healthcare providers. As highlighted in Addiction Science & Clinical Practice:
"Integration of siloed data, made possible given revised regulations, is essential to an efficient hub-and-spoke model of care, which must standardize and coordinate patient care across multiple clinics and departments".
Core Features of Real-Time Systems
Modern systems that enable real-time documentation rely on several important features to centralize and streamline data:
- Centralized Databases: These replace fragmented systems like spreadsheets, paper files, and standalone software. Instead of each program maintaining its own records, all data flows into a single repository, creating a unified source of information.
- Automated Workflows: These ensure that data updates instantly, triggering team notifications and supporting consistent treatment tracking. For example, Denver Health saw a 250% increase in patients tracked as initiating treatment - rising from 562 to 1,411 - after replacing manual methods with automated EHR referral orders between July 2021 and January 2023.
- Standardized Definitions: By using consistent definitions across programs, such as a shared understanding of what constitutes a "treatment episode", data becomes more uniform and comparable. This standardization allows seamless communication across different care settings, from emergency departments to outpatient clinics.
Modern systems also prioritize compliance and interoperability. Features like HIPAA and SOC 2 compliance ensure data security, while standards such as HL7 and FHIR enable recovery centers to exchange information with state benefit systems, referral networks, and compliance platforms. Role-based permissions further safeguard sensitive information, ensuring that team members access only what’s necessary for their roles. This combination of features ensures both efficiency and security in managing client care.
How Recovery Center CRM Eliminates Data Silos
Recovery Center CRM by Bee Purple brings all recovery data together, breaking down silos to give a complete picture of each client's journey. Instead of juggling fragmented records, recovery centers gain a single system that tracks everything - from intake and treatment plans to housing referrals and long-term outcomes. This means case managers and counselors can access all client data instantly.
Justin, a recovery professional using the platform, shares his experience:
"Using this platform, I have the complete profile of a person in recovery with all of our interactions in one place. The amount of time this saves us internally on streamlining administrative processes is huge because having that one centralized location... is so easy to understand and work with".
On average, employees waste 1.8 hours daily (9.3 hours weekly) searching for and gathering information when data isn't centralized. Recovery Center CRM eliminates this inefficiency by offering instant access to comprehensive client profiles, including demographic details, referrals, and interaction histories.
Centralized Documentation for Recovery Programs
Recovery Center CRM replaces scattered record-keeping with a single, reliable database for all client information. Whether the data comes from court referrals, emergency visits, or direct intakes, it flows into one centralized system. This eliminates delays and ensures that staff across programs and locations work with the same up-to-date records.
The platform tracks a wide range of data, such as biopsychosocial assessments, treatment plans, housing status, and employment services. For example, when a client moves from a recovery residence to outpatient treatment, the new team can immediately access the full history - no phone calls, no faxed records, no waiting. This streamlined approach supports timely interventions and coordinated care, which are critical for recovery success. It's particularly helpful for justice-involved clients, as the system ensures a smooth "Warm Handoff" from correctional facilities to community-based care, with medical records and recovery plans following the individual seamlessly.
The platform is also highly adaptable, allowing recovery centers to tailor it to their specific needs. Custom fields, forms, and workflows can be created to fit unique operational requirements. For instance, a recovery housing network might track bed availability and curfew compliance, while a treatment center focuses on clinical progress notes and medication management. All this information is stored in one system, making it easy to coordinate care and automate processes that improve efficiency.
Automated Workflows and Role-Based Permissions
The platform automates repetitive tasks, freeing up staff to focus on client care. Automated workflows handle follow-ups, send reminders for appointments or documentation deadlines, and prioritize outreach efforts. This automation addresses a major challenge in recovery programs, saving staff from hours of manual tracking. Daily reports generated by the system highlight high-need clients, ensuring urgent cases get immediate attention while routine tasks stay on track. Research shows that organizations using integrated data tools are 58% more likely to exceed revenue targets, and data-driven organizations are 162% more likely to significantly outperform their goals.
Role-based permissions enhance security while enabling collaboration. Team members only access the data relevant to their roles. For instance, a peer support specialist might view recovery milestones and housing status, while a clinical supervisor reviews treatment plans and medication records. Automated audit trails track who accesses what information and when, ensuring accountability and HIPAA compliance. This setup allows multiple staff members to collaborate on a single client profile without compromising security or data integrity.
HIPAA and SOC 2 Compliance
Recovery Center CRM meets HIPAA and SOC 2 standards, providing a secure framework for handling sensitive health information. The platform uses end-to-end encryption for both stored and transmitted data, ensuring confidentiality whether data is in the database or shared among authorized users. Automated backups prevent data loss, and strict access controls determine who can view sensitive records.
This compliance framework not only protects data but also supports scalable recovery programs. For example, state health departments can use aggregated data to demonstrate the effectiveness of public funding, prepare reports for federal grants, and present materials for legislative budget hearings. All of this happens under strict role-based permissions, allowing agencies like courts, health departments, and housing providers to share data securely.
Poor data management costs organizations an average of $12.9 million annually. Additionally, failing to maintain proper data governance across siloed systems can lead to costly HIPAA and SOC 2 penalties. By centralizing data in a managed CRM, recovery centers reduce risks by eliminating vulnerable, outdated repositories that could be targeted by ransomware. This robust compliance infrastructure ensures that as recovery programs grow, they maintain the security and governance standards necessary for long-term success.
sbb-itb-ce23a48
Benefits of Real-Time Documentation for Recovery Programs
Real-time documentation builds on the strengths of centralized data by improving clinical decisions, streamlining operations, and enabling long-term tracking. The ability to access and act on data instantly allows for quicker responses to client needs, ultimately enhancing care and outcomes.
Better Clinical Decision-Making
When counselors and case managers have immediate access to the latest client information, they can adapt treatment plans as circumstances change. For example, Denver Health’s integration of substance use disorder data replaced outdated manual spreadsheets with standardized referral orders. This shift resulted in a 250% increase in patients tracked and boosted 90-day retention rates from 45% to 74%.
With real-time access to comprehensive client histories - including biopsychosocial assessments, housing status, and medication details - staff can spot potential warning signs early. This allows for timely interventions that can prevent crises and save lives. Marsha Stone, JD, LCDC, Founder and CEO of Foundation Stone, highlights the importance of this approach:
"Real-time data allows healthcare providers to monitor and adjust treatment plans promptly based on the latest information, leading to more effective and personalized care".
Easier Operations and Reporting
Centralized documentation eliminates the inefficiencies of chasing down records through phone calls, faxes, or emails. Platforms like Recovery Center CRM automate routine tasks like follow-ups, appointment reminders, and tracking documentation deadlines, giving staff more time to focus on clients.
Supervisors benefit from automated dashboards that provide a real-time view of caseloads, tasks, and patient statuses - all without relying on external databases. This streamlining simplifies compliance reporting for funding sources like Opioid Settlement Grant Funds. For example, state health departments can use aggregated data to showcase the effectiveness of public funding during legislative budget hearings. Built-in role-based permissions ensure HIPAA compliance while maintaining data security.
Long-Term Outcome Tracking
Real-time documentation doesn’t just improve immediate care - it also supports sustained recovery by tracking progress over time. This is critical, as fewer than 42% of individuals entering drug or alcohol treatment complete their programs. Platforms like Recovery Center CRM follow clients from intake to discharge and beyond, helping identify where programs succeed and where additional support is needed.
One standout feature is the Global Recovery Score, which combines resilience factors (like gratitude and hope) with pathology factors (such as depression and anxiety) to provide a well-rounded view of client progress. This long-term visibility allows programs to make informed adjustments that improve retention rates and demonstrate success to funders. For justice-involved clients, the system ensures continuity of care, tracking progress from correctional facilities to community programs. This reduces the risk of individuals falling through the cracks during critical transitions.
Steps to Implement Real-Time Documentation in Recovery Centers
Transitioning to real-time documentation involves evaluating current systems, adopting the right technology, and rolling out staff training in structured phases.
Review Current Data Management Practices
Begin by identifying inefficiencies in how your organization manages data. Common warning signs include clinicians repeatedly asking clients for the same information, staff manually transferring data between systems, or relying on outdated methods like spreadsheets or fax machines to share records. Systems older than a decade, those requiring complex custom coding for integration, or platforms lacking support for interoperability standards like FHIR or HL7, are strong indicators that your infrastructure may need an upgrade. Globally, fragmented systems cost the healthcare industry around $3.1 trillion each year due to inefficiencies and gaps in care.
Conduct a thorough audit of your data quality. Look for duplicate records, inconsistent analytics, and broken workflows across intake, clinical care, and billing. Poor data management costs companies an average of $12.9 million annually, and approximately 80% of businesses face challenges with data silos. Document your current workflows in detail - this baseline will help measure improvements once new systems are in place.
| Assessment Area | Key Indicators of Inefficiency |
|---|---|
| Clinical Workflow | Excessive time spent reconciling data; repeated client queries. |
| Data Integration | Outdated systems; reliance on custom coding; lack of FHIR/HL7 support. |
| Administrative | High costs from repeated tests; long billing cycles; frequent data errors. |
| Data Quality | Duplicate records; inconsistent analytics; departmental information gaps. |
With a clear understanding of the issues, the next step is to modernize and centralize your data management system.
Adopt Recovery Center CRM for Centralized Documentation
The Recovery Center CRM is designed to break down data silos by consolidating all client information - covering everything from intake forms and biopsychosocial assessments to medication tracking and housing status - in one secure platform. This ensures that staff across clinical, administrative, and case management roles have access to the same up-to-date information.
The system automates routine tasks like appointment reminders, follow-ups, and documentation deadlines, saving time and reducing errors. Role-based permissions safeguard sensitive information, ensuring compliance with HIPAA and SOC 2 standards. For justice-involved clients, the CRM tracks their progress from correctional facilities to community programs, ensuring seamless transitions and continuity of care.
Scalability is a major strength of this platform. State health departments can use aggregated data for budget hearings, while individual recovery centers benefit from real-time dashboards that provide insights into caseloads, task completion, and client progress. Its cloud-based infrastructure can grow with your organization, making it suitable for both single-location centers and statewide networks.
Once the system is implemented, focused training and ongoing performance monitoring will drive its success.
Train Staff and Monitor Progress
A structured 90-day training plan ensures smooth adoption:
- Days 1–30: Define key performance indicators (KPIs), configure workflows, and train a core group of "super-users."
- Days 31–60: Pilot the system with a small group of clients, conduct daily check-ins, and refine processes based on initial feedback.
- Days 61–90: Expand the system to the entire facility and share performance dashboards to highlight progress.
Training should be tailored to specific roles. Clinicians can focus on real-time treatment planning, while administrators master reporting and compliance. Simulations for tasks like intake and medication reconciliation help staff gain confidence. Cross-department shadowing can further enhance system fluency. Organizations with integrated systems report a 42% boost in clinical workflow efficiency and a 35% drop in medication errors.
Weekly cross-functional meetings can help leadership review metrics, share success stories, and address challenges. Displaying real-time analytics in common areas allows staff to see how their work directly impacts client outcomes. Success is evident when siloed reporting shifts to integrated data sharing, enabling agencies to collectively report on client experiences.
"Each community has unique partnerships, infrastructure, policies, and procedures that need to be considered when developing data sharing efforts." – California Health Care Foundation
Track metrics such as data retrieval times, documentation completion rates, and staff time saved. For instance, unified platforms have been shown to reduce diagnostic errors by 33%, improve patient satisfaction by 28%, and enhance emergency response times by 47%.
Conclusion
Data silos create significant hurdles in recovery programs, wasting clinicians' time and obstructing access to vital information. Real-time documentation breaks down these barriers by generating a unified, secure record that includes intake forms, treatment plans, housing details, and medication. Studies consistently highlight how integrated systems improve patient tracking and retention rates compared to fragmented methods.
With real-time processing, recovery programs can make decisions based on up-to-date information rather than outdated records. Automated workflows replace time-consuming manual data entry, reducing administrative processing times by 50%. This allows staff to shift their focus from paperwork to client care, improving overall efficiency and outcomes. These operational advantages naturally connect to the role of CRM systems in centralizing client data.
Recovery Center CRM builds on these benefits by consolidating all client data into one platform, enhancing recovery outcomes. By eliminating long-standing barriers to data sharing, the system offers a HIPAA- and SOC 2-compliant framework. Role-based permissions ensure data security while enabling smooth collaboration across clinical, administrative, and case management teams. For state health departments and justice-involved populations, the platform tracks long-term outcomes and provides the aggregated data needed for budget hearings and grant compliance.
The stakes are high. Fragmented systems cost the global healthcare sector billions each year, emphasizing the pressing need for real-time, unified documentation in recovery programs. Centers that adopt these systems gain the tools to deliver comprehensive care, ease administrative workloads, and demonstrate measurable results - reshaping how they support individuals on their recovery journey.
FAQs
How does real-time documentation enhance care coordination in recovery programs?
Real-time documentation plays a key role in improving care coordination by offering up-to-date information that helps recovery teams make informed decisions quickly. This approach breaks down data silos, giving a more comprehensive view of each person’s progress throughout their recovery journey.
When crucial data is centralized, recovery programs can improve communication between providers, monitor long-term outcomes, and fine-tune treatment plans when necessary. The result? More tailored care and improved outcomes for individuals working toward recovery.
How does Recovery Center CRM help eliminate data silos in recovery programs?
Recovery Center CRM simplifies the management of recovery programs by bringing all documentation together in one place. This includes everything from individual recovery plans and demographic details to interaction histories, ensuring that information is organized and easy to access. By centralizing data, it eliminates the frustration of dealing with scattered records.
The platform helps track recovery progress, schedule appointments, and send reminders to keep care consistent and on track. Its advanced data analytics dig into health records, treatment results, and behavioral trends, offering insights that connect the dots between different aspects of the program.
With tools like customizable reports and smooth data sharing, Recovery Center CRM eliminates barriers caused by fragmented information. It creates a more connected, data-driven system that improves communication, coordination, and long-term recovery efforts.
How can recovery centers protect client data while using real-time documentation systems?
Recovery centers can safeguard client information by utilizing secure, HIPAA-compliant systems. These systems should include features like encryption, strict access controls, and regular security audits. Such measures help ensure that sensitive data remains protected and is only accessible to authorized individuals.
To strengthen security further, centers should adopt controlled access protocols, train staff regularly on privacy and confidentiality practices, and keep detailed audit logs to monitor who accesses or modifies data. Following federal regulations such as 42 CFR Part 2 is also critical, as it ensures compliance with confidentiality rules specific to substance use disorder records. This not only protects data but also builds client trust.
By combining strong security practices with adherence to regulations, recovery centers can confidently use real-time documentation systems to support recovery efforts while keeping client information safe.

